43 M with abdominal distension
- Get link
- X
- Other Apps
A 48 years old male , bus driver by occupation presented to opd with chief complains of huge abdominal distension.
CHIEF COMPLAINTS
Abdomen distension since 4months
Swelling of both legs since 2 months
Decreased urine since 1 month
DAILY ROUTINE
5 AM : wakes up
5:30 AM: haves green tea with two biscuits and beetle nut
6AM : starts from his house on bicycle and covers about 5kms in 15 minutes
6:30 AM : He starts from silguri to tinsukia which is around (1000) kms
9am:- He halts his bus for breakfast where he takes rice and dal with two pieces of fish and starts again
1pm :- He stops the bus for lunch (rice and dal with two pieces of small fish)
1-5pm :- Rest(his codriver takes over)
5pm:- Cup of milk with biscuits and starts his journey
10pm:- Stops for dinner, has rice and dal with fish and starts driving up to 6am
6am:- Halts and takes biscuits with tea and beetle nuts
Afternoon:- He reaches tinsukia and sleeps
8pm:- 600ml of desi beer with fishes
10pm:- sleeps
5am:- He starts up for siliguri
He takes round trips two times a week.
He used to smoke beedi and gutkha amid his journey but never took alcohol cause of strict police.
He is into this profession since 28 years and took last trip 3 days before so that's the last alcohol intake.
He denied taking alcohol since few months.
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 4months ago. Following his daily routine he was cycling to earn his bread at around 6am. Few of his friends noticed that he is getting fat and obese but cause of his healthy life style he didn't pay much heed. Within 2-3 weeks few more people noticed that he is getting protruded abdomen which doesn't seems to fit in the puzzle according to his general physique. Some said that he has jaundice and sent him to a quack who seems to cure jaundice Within couple of hours. Although his so called jaundice didn't get cure but that quack said him that he got water in his belly and need to take proper medical care. And after few investigations he presented to our hospital with chief complaints of distended abdomen which is insidious in onset gradually progressive associated with decreased appetite since then.
Bilateral pedal edema extending upto knee since 2 months , pitting type increased on walking and relieved with rest
Decreased urinary output since 1 month
No h/o fever, cough, breathlessness.
No h/o drowsiness, loss of consciousness, palpitations, orthopnoea,pnd ,abdominal pain, fever,nausea vomiting.
PAST HISTORY :
No H/O similar complaints in past.
No H/O DM HTN TB asthma epilepsy CVA CAD.
PERSONAL HISTORY :
Occupation:Bus driver
Patient is married .
Patient takes mixed diet and has a decreased appetite .
Sleep : Regular
Bowel movements are regular and bladder movements are reduced .
Consumes 600ml alcohol occasionally and stopped 1 year back.
smokes beedi 1 pack per day and stopped 3 months back
GENERAL PHYSICAL EXAMINATION:
Patient is conscious ,coherent and cooperative and well oriented to time, place , person.
Patient was examined in a well lit room after taking their consent.
Patient is severely undernourished with marked sarcopenia
Pallor- present
Icterus -absent
Cyanosis-absent
Clubbing-absent
Generalised Lymphadenopathy-absent
Edema-bilateral pedal edema present
VITALS
Temperature : 98.3℉
PR : 90 beats per minute
BP : 100/70 mm of Hg
RR : 22 cycles per minute
SpO2 : 96% room air
SYSTEMIC EXAMINATION
Per abdomen -
Abdominal girth- 93-->91cm
Inspection-
Abdomen is distended , flanks are full, skin is stretched , no visible peristalsis , equal symmetrical movements in all quadrant’s with respiration
Palpation -
No local rise of temperature, no tenderness
All inspectory findings are confirmed by palpation, no rebound tenderness, gaurding and rigidity.
No tenderness , No organomegaly
Fluid thrill present
Percussion:
Shifting dullness present
Auscultation:
Bowel sounds heard
CVS : S1 and S2 heart sounds heard
CNS: No focal neurological deficits
Cranial nerves,motor and sensory functions intact.
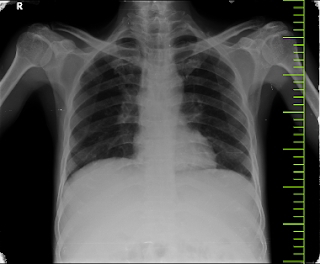
RR: BAE Present, normal vesicular breath sounds heard,no adventitious sounds
shape of the chest: normal
trachea appears to be central
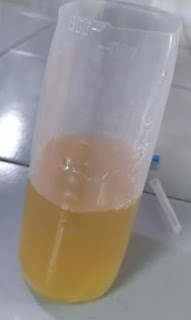
Ascitic fluid
PHES test
Interpretation :
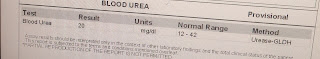
INVESTIGATIONS
1. Complete Urine Examination
2. Anti-HCV Antibodies
3. GRBS
4. Blood urea level
5. HBsAg
6. Hemogram
7. HIV Rapid test
8. LFT
9. Serum Creatinine
10. APTT
11. Bleeding and clotting time
12. Prothrombin time
Ascitic tap -
Appearance - clear , yellow coloured
SAAG - 1.65 g/dl
Serum albumin - 2.0 g/dl
Asctic albumin - 0.35 g/dl
Ascitic fluid sugar - 104mg/dl
Ascitic fluid protein - 0.7 g/dl
Ascitic fluid amylase - 17 IU /L
LDH : 143 IU/L
Cell count- 50 cells
Lymphocytes nil
Neutrophils 100%.
TREATMENT :
Tab LASIX 40 mg PO BD
Syp. Lactulose 10 ml PO HS
Strict Alcohol abstinence .
- Get link
- X
- Other Apps